Serotonin is NOT the Happy Hormone
Even after the largest study ever on serotonin published in 2022 destroyed the myth that low brain serotonin causes depression, the fiction that serotonin is the ‘happy hormone’ still persists.
In today’s article I’ll demonstrate serotonin’s primary role in the body, how elevations in serotonin are more likely leading to mood disorders, and how too much serotonin is anti-metabolic.
TLDR:
1. The serotonin theory of depression has been soundly destroyed and its more likely that elevated serotonin is problematic
2. Serotonin’s primary function in the body is for intestinal motility. Gut dysfunction (of any kind) causes an increase in intestinal serotonin which translocates to the brain via the vagus nerve
3. Most everyone with mood disorders also has an underlying gut issue
5. SSRI’s cause gut dysbiosis, sexual dysfunction, will wreck your metabolism, and were developed out of early CIA research on LSD
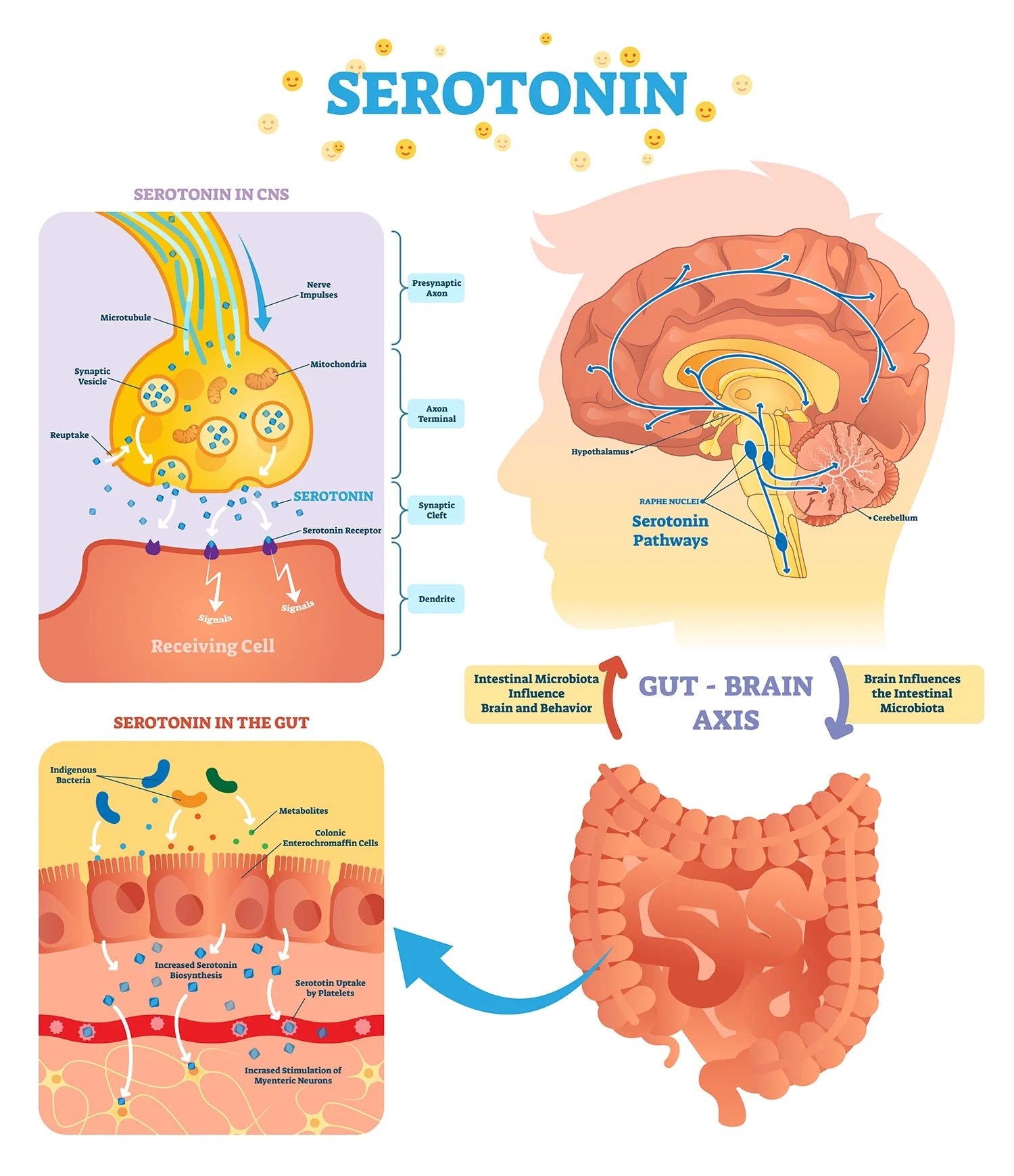
Although long known as the “happy hormone”, the primary role of serotonin is for gut motility. 95% of your serotonin is made by cells embedded in the gut ling called Enterochromaffin cells. As digested food comes into contact with these cells, they’re stimulated to produce serotonin and the serotonin acts on the smooth muscle neurons that then contract creating motility.
Gut irritation from pathogenic bacteria, parasites, allergenic foods, plant anti-nutrients, or artificial ingredients can increase serotonin release as part of the immune response. When coming into contact with the enterochromaffin cells, these irritants cause a high production of serotonin leading to higher motility. For reference, the last time you had food poisoning it was the increased release of serotonin that caused the diarrhea.
Gut-based serotonin is easily able to affect the brain via the vagus nerve and vice versa. GI dysfunction is often a precursor to disturbances in mood as more than half of people with functional gastrointestinal disorders (FGIDs) also have depression or anxiety conditions.
Gut irritants stimulate enterochromaffin cells in the intestinal epithelium to produce more serotonin (5-HT) via the enzyme tryptophan hydroxylase 1 (TPH-1). In small intestinal bacterial overgrowth (SIBO), there is increased expression of TPH-1 mRNA in the small intestinal mucosa, leading to higher serotonin production.
Gut dysbiosis can affect the metabolism of tryptophan, the precursor to serotonin, increasing serotonin production. Inflammation or irritation affects the function of the serotonin reuptake transporter (SERT), leading to increased extracellular serotonin. By the way, selective serotonin reuptake inhibitors (SSRIs) ALSO reduce SERT activity, increasing available serotonin. Funny how gut problems and SSRIs both increase serotonin but we’ll get into SSRIs a bit later…
Another pathology that arises with increased serotonin is insomnia. Serotonin is a daytime hormone produced as a result of eating and should cycle down during sleep. Increased gut-based serotonin can prevent sleep onset and REM. If you have gut problems, mood problems and sleep problems the issue is almost certainly elevated serotonin due to a gut irritant.
The largest study ever on serotonin was published in 2022 and firmly debunked the pharma-based claim that low serotonin causes depression.
The review included 17 studies: 12 systematic reviews and meta-analyses, 1 collaborative meta-analysis, 1 meta-analysis of large cohort studies, 1 systematic review and narrative synthesis, 1 genetic association study, and 1 umbrella review
Key results:
No consistent evidence of there being lower levels of serotonin in people with depression compared to people without depression
Artificially lowering serotonin levels did not produce depression in hundreds of healthy volunteers
Genetic studies involving tens of thousands of patients found no difference in serotonin-related genes between people with depression and healthy controls
Another study found that overt SSRI treatment (where patients knew they were receiving an SSRI) was superior to covert treatment, resulting in almost a fourfold higher rate of responders. Even though placebo seems to account for effect in SSRIs, there are some people that benefit from SSRIs.
In order to understand how this benefit occurs we need to look at the anti-metabolic effects of serotonin.
The Anti-Metabolic Effects of Serotonin
Serotonin is part of a stress response and upregulated by cortisol
It inhibits energy production of the mitochondria of liver and brain by down-regulating oxidative phosphorylation
It is involved in driving obesity, insulin resistance and fatty liver
So why do SSRIs work for the minority of its users?
The study above makes a few clarifying points about the metabolic impact of the serotonergic system.
Serotonin transmission is elevated in multiple depressive phenotypes, including melancholia, which is associated with sustained cognition
The serotonergic system evolved to regulate energy. SSRIs, by increasing extracellular serotonin, disrupt energy homeostasis and can worsen symptoms during acute treatment
Symptom reduction from SSRIs is not due to their direct pharmacological properties, but rather the brain's compensatory responses to restore energy homeostasis. This explains the therapeutic delay of SSRIs and the benefits for the non-placeboed
The history of SSRIs is a dark and winding road. It was spawned after years of CIA MkUltra experimentation on civilians using LSD. It turns out that LSD is the most potent anti-serotenergic compound known. And when the military tested LSD as a nootropic for soldiers, they got non-compliance and disobedience.
In 1987 the first major SSRI, Prozac, was released by Eli Lilly. The German BGA (like the FDA) rejected Eli Lilly’s approval for Prozac because in Lilly’s own studies they demonstrated suicidal tendencies. Later, the Boston Globe in 2000 reported on this having obtained access to Lilly’s original studies stating “previously non-suicidal patients had a five-fold higher rate of suicide and suicide attempts than those on older antidepressants and three-fold higher than placebo”.
In 2004 after years of battle, the FDA was finally forced to force manufacturers to include a black box warning stating: “Antidepressants increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults under 25 years old with major depressive disorder (MDD) and other psychiatric disorders.”
On top of that and the gut disruption caused by SSRIs, they also cause sexual dysfunction in up to 65% of its users.
If you’d like to dig deeper into the history of LSD and SSRIs check out the documentary above. Be warned, it will not make you happy.
What’s important to remember here is that health and wellbeing are the result of sufficient energy production aka good metabolic function so that means:
Fix your gut
Optimize your mitochondria
Restore glucose metabolism
To your health, Jonathan