Anemia & Iron Overload: Two Sides of Iron Disregulation
Iron is a necessary mineral for many proteins in the body most notably hemoglobin, the protein responsible for transporting oxygen from the lungs to your cells for mitochondrial use during energy production. Anemia refers to a deficient amount of hemoglobin that’s usually blamed as iron deficiency. Many men and post-menopausal women are negatively affected by excess iron that causes severe oxidative stress and aging. Iron disregulation is a common and important factor in lowered energy production and accelerated aging.
In today’s article I’ll run though iron dynamics, the pervasiveness of anemia and Iron Overload (IO), and solutions to rebalance iron.
TLDR:
Iron is highly oxidative and must be housed in proteins like hemoglobin, transferrin and ferritin to prevent oxidative damage as well as sequester it from pathogens that use it as fuel.
Ceruloplasmin is a unique copper-based protein this is responsible for regulating iron through a process that recycles 90% of the iron in hemoglobin. Anemia develops with lowered ceruloplasmin levels.
Lipofuscin is the destructive, brown-pigmented by-product of free iron reacting with polyunsaturated fats that damages skin, heart and brain cells.
Beef liver is the best food for healing anemia and blood donation is the best way to lower iron if overloaded.
Iron is a key component of hemoglobin, the protein in red blood cells responsible for transporting oxygen from the lungs to cells throughout the body. About 70% of the body's iron is found in hemoglobin. Each hemoglobin molecule contains four iron-containing heme groups that can bind oxygen molecules.
Roughly 10% of iron is also present in myoglobin, a protein that stores oxygen in muscles and facilitates oxygen diffusion to mitochondria during periods of increased metabolic activity.
Heme proteins in the electron transport chain, specifically Cytochrome c, Complex III and Complex IV, contain iron as a way to pass electrons down the chain to oxygen (from your breath) to make water. The iron pool in enzymes represents about 5% of total.
And the remaining 15% can be found the proteins ferritin, hemosiderin and transferrin. In total, men have about 4 grams of iron and women 3.5 grams.
Iron is also what makes your blood red. More heme saturation of oxygen makes blood brighter and less heme saturation of oxygen makes it darker.
The human body makes over 200 billion red blood cells/day and 25 mg of iron are required for this process called erythropoiesis. 24 of those 25 mgs in healthy iron regulation come from the reticuloendothelial system (RES) aka the iron recycling system. Because of this recycling, only 1mg of iron is required from our diet yet the average American diet gets 10-20mg/day. I personally average 11mg/day.
When more comes in through the diet than bound to proteins, the body stores it in the liver, the endocrine glands (ovaries and testes), heart, brain and joints. Iron is the third most oxidative element on the planet after fluorine. Too much unbound iron in tissues leads to production of hydroxyl free radicals which are highly damaging to healthy tissue. There is no enzymatic process to breakdown iron though we do lose about 1mg/day in stool. Because of these processes, unless you’re bleeding regularly you’re likely storing iron in aforementioned tissues.
A suppressive hormone produced by the liver called hepcidin regulates dietary iron absorption in the small intestine. When iron levels are high, hepcidin production increases reducing iron absorption from the gut. When iron levels are low or during increased erythropoiesis, hepcidin production decreases allowing more iron to be absorbed and released into circulation.
Theoretically, if your iron status is sufficient the unabsorbed iron is trapped iron in enterocytes then excreted through feces when they turnover. I say theoretically because it is very common for people on a carnivore diet to become iron overloaded as seen in hemoglobin and ferritin levels. There appears to be an upper limit to hepcidin’s effects. Beyond this, accumulated iron in enterocytes is theorized as one cause of bacterial overgrowth in the gut as high iron environments provide fertile terrain.
The most common genetic disorder among humans is hemochromatosis caused by mutations in the HFE gene. Hemochromatosis effectively prevents hepcidin from working and thus massively increasing iron absorption. Regardless of your HFE gene status or if your eating carnivore, its important to at least test hemoglobin and ferritin to determine your status because most people tend to have some form of iron disregulation.
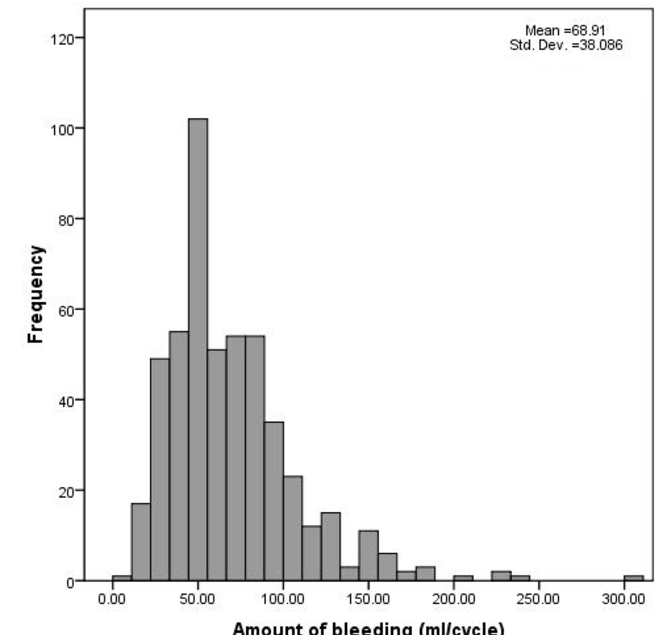
The average cycling woman loses 450ml/blood per year equal to 1 blood donation. For cycling women, the blood loss (iron loss) combined with lack of dietary copper, retinol and ceruloplasmin production is the perfect formula for anemia. In this case, if you get your iron status tested through a doctor they will most likely recommend supplementing iron (non-heme) which may temporarily improve symptoms but will eventually return when you’re done supplementing. This is because the problem isn’t caused by lack of dietary iron, it’s that the recycling system is offline due to lack of functional ceruloplasmin. Iron recycling is regulated by ceruloplasmin and relies on copper and retinol to form itself.
The same high absorption that I mentioned with hemacromatosis and carnivore dieters can occur in cycling women but without the increase in iron markers. This is also due to lack of functional ceroluplasmin. After looking at 50 healthy, cycling women’s iron panels I have never seen a ferritin level above 100 even when eating red meat.
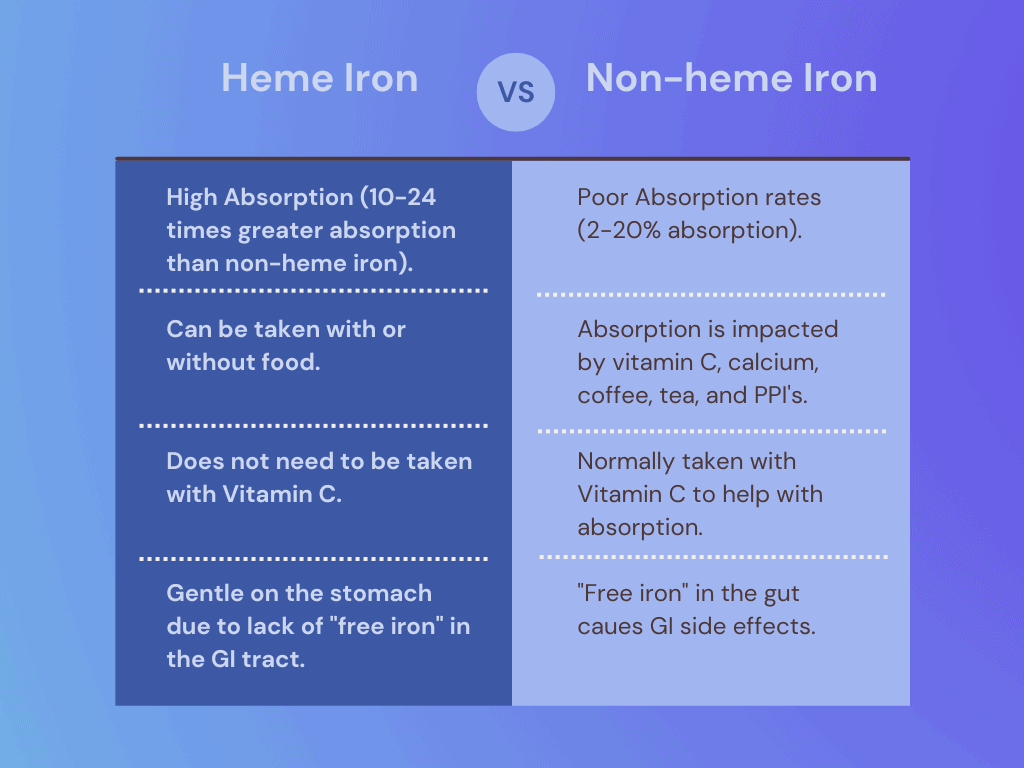
There are two types of dietary iron - heme and non-heme. Heme iron exists in animals and non-heme in plants. The absorption of heme iron is significantly higher than non-heme and should be a focus if you’re diagnosed with anemia. In a addition to heme-iron found in organ and muscle meat, there are high amounts of Folate and B12 which are necessary for the formation of hemoglobin.
Beef liver is the perfect food for restoring iron function as it contains vitamin a (retinol), copper, heme-iron, folate and B12. I’ve seen many people, especially menstruating women recover from anemia when increasing beef liver consumption and supplementing copper. Hypothyroidism is common with anemia. Both of these together significantly lower energy metabolism in the body. Do not supplement with non-heme iron.
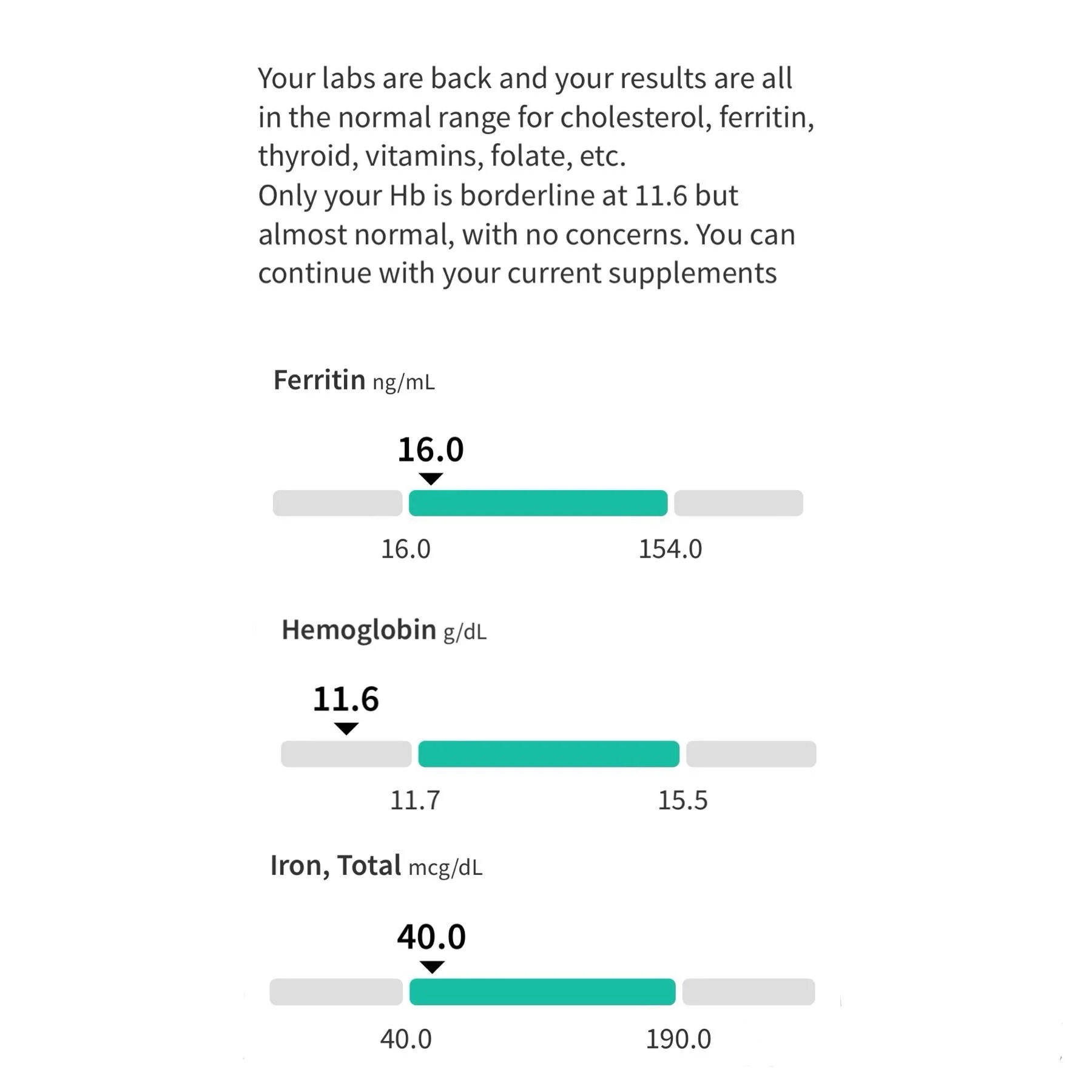
Ideal Hemoglobin Men 14-15 g/dL, Women 13.5-14.5 g/dL
Ideal Ferritin 45-79 ng/mL - I aim for 50 ng/mL
Both of these blood tests are easy to order yourself through Marek Health.
If you’re below these values and tend to trend downwards, focus on eating liver (~ 6 oz/week) and supplementing copper bisglycinate at 3mg/day.
If you’re above these ideal values and trend upwards, this means you’re iron overloaded and should donate blood. Since I tend to accumulate iron, I donate blood when my ferritin reaches 80-100. This occurs approximately every 6 months however I spent almost year doing aggressive phlebotomy (not recommended) to move my ferritin from 185 to 50. More on blood donation in a bit…
Free iron acts as a catalyst in the oxidative processes leading to lipofuscin formation aka liver spots. When free iron reacts with polyunsaturated fats, these dark pigments emerge. When skin cell are comprised of primarily from dietary PUFA, UV light from the sun can also cause this along with easy sunburning. This lipofuscin is far worse when it occurs inside the body, particularly in heart cells and neurons.
Lipofuscin accumulation in the heart is linked to heart disease and cardiac aging. It accumulates in cardiomyocytes over time, with its accumulation rate positively correlating with chronological aging. It’s associated with oxidative stress and mitochondrial dysfunction, which are known contributors to heart disease.
Lipofuscin accumulation in the retina is a risk factor for macular degeneration, accumulation in the brain with neurodegenerative diseases like alzheimers and dementia.
Another detrimental reaction occurring between free iron and PUFA is called ferroptosis. Ferroptosis contributes to the development of atherosclerotic plaques by causing endothelial dysfunction and lipid peroxidation.
Knowing the negative systemic impacts of both PUFA and free iron, managing these two are critical for healthy aging. I’ve already covered the benefits of reducing PUFA below 5g/day and increasing healthy saturated fats stabilize cell membranes, particularly mitochondrial membranes.
Additionally, it’s very important to remove excess iron from the body so it doesn’t cause lipofuscin and ferroptosis in the liver, heart and brain. Considering that the average American gets roughly 15 mg though their diet, it accumulates relatively quickly.
Blood donation and phlebotomy are the best way to remove excess iron. A standard blood donation will remove 450-500 ml of whole blood, lower ferritin about 40 points, and remove approximately 200-250 mg of iron. Recently I consulted a 50 yo man that had a ferritin of 298. To reduce his ferritin to 50, that’s 7-8 donations, every 2 months for 14-16 months. The most common symptom I hear from people with IO is “fatigue” and the most common remark I hear to donating blood is feeling “lighter” and more “energetic”.
If you’re already low hemoglobin and ferritin (many menstruating women are), blood donation can severely worsen symptoms of anemia. Generally speaking if your a man or postmenopausal woman eating meat, you can and should be donating.
Blood donation is also a way to remove toxins from your body including microplastics and per- and polyfluoroalkyl substances (PFAS), commonly known as "forever chemicals." Some groups are at high risk for PFAS namely firefighters and those exposed to fire retardents, foams and extinguishers. This is particularly relevant now in the wake to the horrific LA fires. PFAS are linked to birth defects, infertility, many cancers, and generational defects. Plasma donation was found to remove 30% of PFAS from blood over 12 months, more than twice the amount of whole blood donation. Plasma donation (no red blood cells) is a good option for menstruating women who are anemic.
Blood donation has been associated with a reduced risk of cardiovascular disease (CVD), primarily due to its effect on lowering iron levels in the body. A Finnish study of 2,862 men found that blood donors had an 88% reduced risk of acute myocardial infarction compared to non-donors over a 9-year follow-up period.
One hypothesis for women generally living longer than men is due to iron depletion by the menstrual cycle. A large study of 1,182,495 blood donors found a 7.5% decrease in mortality risk per additional annual donation, after adjusting for demographic factors and the healthy donor effect.
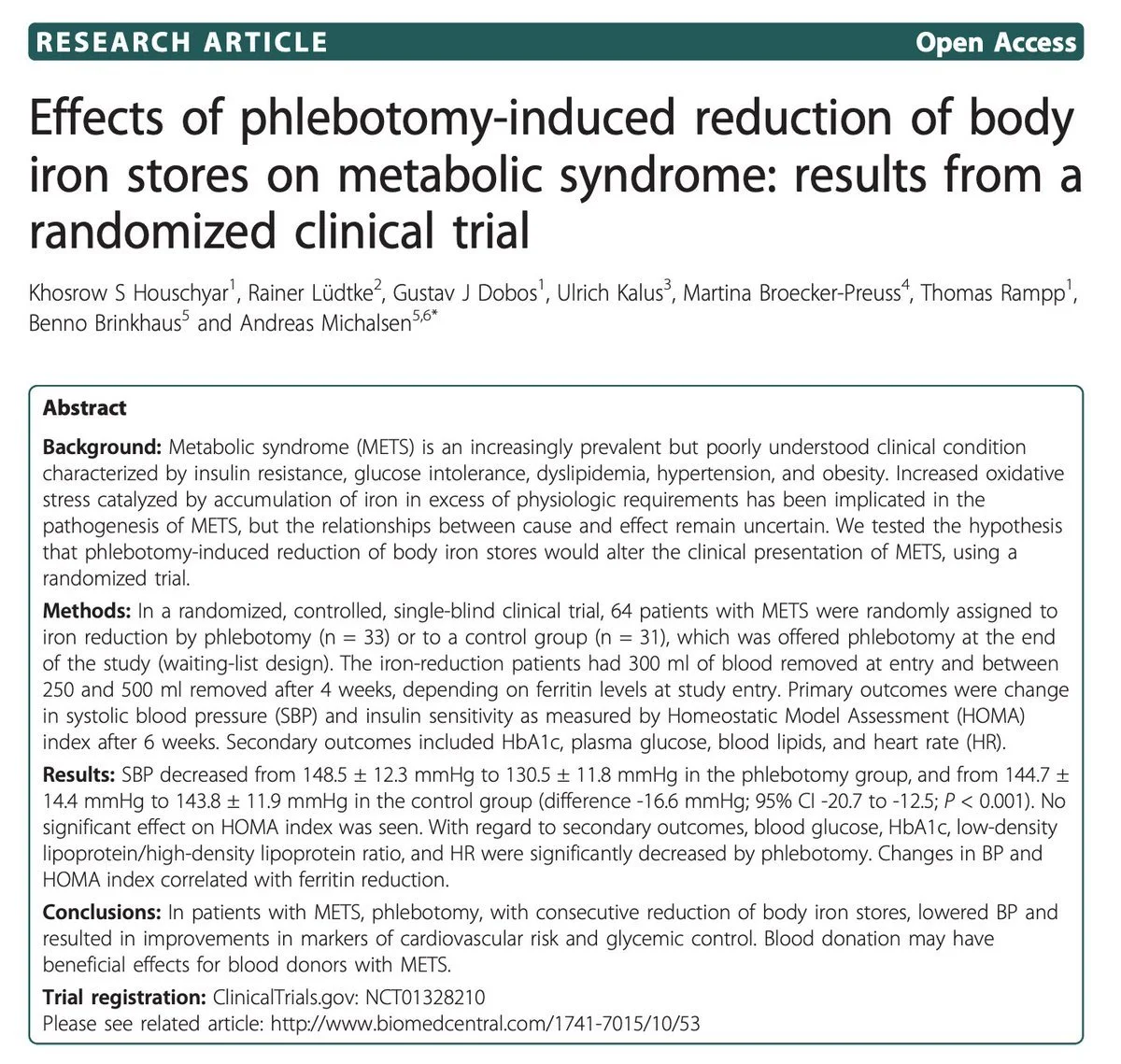
Blood donation improves metabolic syndrome. This study showed donating blood three times improved insulin sensitivity and decreased insulin secretion. Iron accumulation (especially in liver) can drive oxidative stress and inflammation leading to insulin resistance.
This study showed two sessions of phlebotomy significantly lowered blood glucose, HA1C, LDL cholesterol and heart rate.
Since microbes feed on free iron, there is a constant battle by our bodies to sequester iron in proteins so bacteria don’t have access to them. Many pathogenic bacteria require iron for DNA synthesis, electron transport, and other metabolic processes. Transferrin and ferritin are part of our innate immunity sometimes called nutritional immunity. During infection, ferritin expression increases, particularly in response to inflammatory signals. This is why its also known as an “acute phase reactant”.
The importance of these proteins in nutritional immunity is highlighted by studies showing that individuals with iron overload disorders are more susceptible to infections.
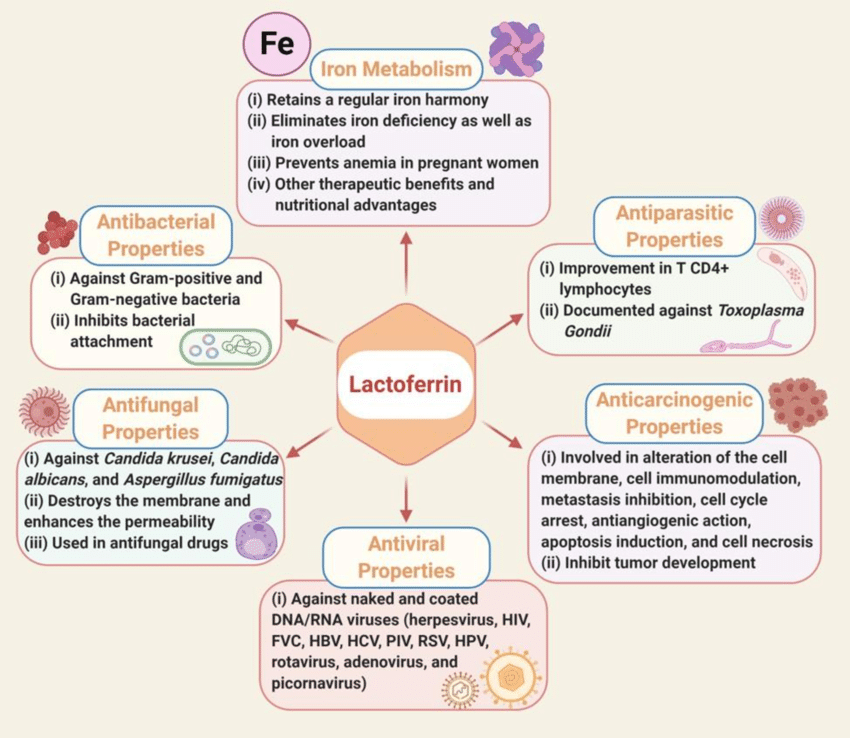
Lactoferrin's antimicrobial activity, a molecule contained in colostrum and milk, is largely due to its ability to bind free iron, depriving microbes of this essential nutrient. Lactoferrin's affinity for iron is 250-300 times higher than transferrin, the main iron transport molecule in the human body. In fact, this is a core protective mechanism for breastfeeding infants against pathogens. Taking lactoferrin (or Colostrum) is also a potent tool in lowering bacterial loads in the gut in cases of SIBO or dysbiosis.
To your health,
Jonathan
This is for informational purposes only and should not replace professional medical advice. Consult with your physician or other health care professional if you have any concerns or questions about your health.