How to Fix Your Gut, part 1
Hippocrates, the ancient Greek physician and father of modern medicine, famously stated that “all disease begins in the gut.” In the last decade this statement has renewed meaning with over 40,000 publications listed in PubMed (60% of these in the last 3 years) on the microbiome demonstrating its impact on metabolic disease, cognitive decline, mental health disorders, and autoimmunity.
What has also manifested recently are the myriad of ways to restore gut health with some of them working for others but not you and vice versa. The reason for these inconsistencies lies in your unique gut status.
In this series we’ll seek to understand how the gut functions, it’s major disrupters and a few approaches to healing it.
TLDR:
1. LPS is arguably the worst assault coming from your gut and lowering it is critical to restoring proper energy metabolism
2. Seed oils, stress hormones, pesticides, and high fat diets are contributing factors to elevations in LPS
3. The migrating motor complex is a built-in mechanical wave that moves bacteria from the small intestine back to the colon where is belongs
4. Hypothyroidism and plant defense chemicals are often overlooked causes of gut distress
The first point to grasp is the toxicity of something called lipopolysaccride (LPS) aka Endotoxin. LPS is a molecule contained in the cell wall of gram-negative bacteria. It is a potent activator of inflammation and often used experimentally to induce inflammatory responses in cells or animal models. LPS also directly damages the mitochondria, produces ROS and induces cell apoptosis. In other words, LPS shuts down energy production in the cell. An overgrowth of gram-negative bacteria, whether in the small or large intestine, will cause metabolic “endotoxemia” that leads to insulin resistance, obesity and CVD.
The gram-negative bacteria in the gut tend to be the “opportunistic” or “pathogenic” bacteria. In a healthy microbiome, they are kept in check through competitive inhibition by the good guys known as “probiotics.” If the microbiome architecture gets disrupted opportunistic and pathogenic gram-negatives can overgrow leading to elevated LPS. LPS is a major contributor to fatty liver, SIBO and Dysbiosis.
There are 3 categories of bacteria in your gut - aerobes, facultative anaerobes and obligate anaerobes. Aerobes live from the mouth to stomach in this oxygen rich environment. In a healthy stomach, the acid provides a barrier that prevents the passing of any outside microbes into the small intestine. From the duodenum through the ileum there is a decreasing amount of oxygen and the colon should be completely oxygen free. This terrain allows for different types of bacteria to exist at different locations.
From the stomach through the small intestine bacterial counts should be orders of magnitude lower that of the mouth or colon.
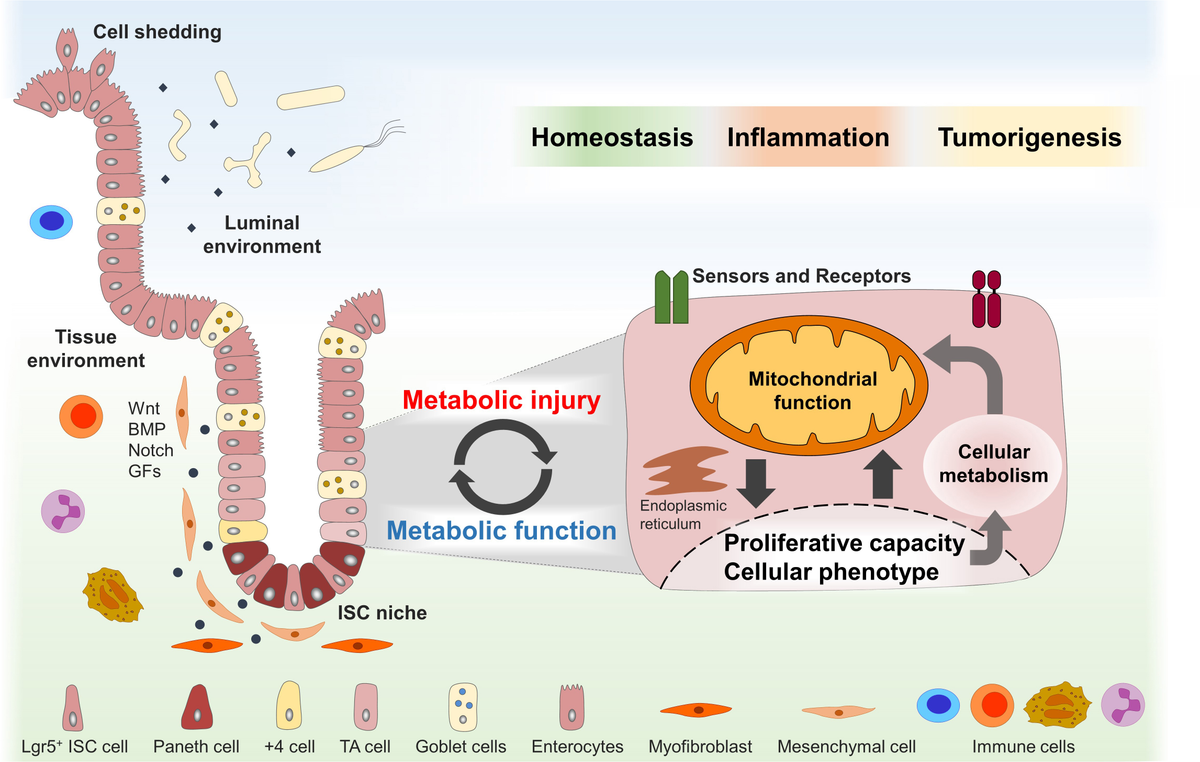
There are two important functions that fail in people with gut issues that maintain proper oxygen concentrations and bacterial counts - the migrating motor complex (MMC) and good mitochondrial energy production of intestinal cells.
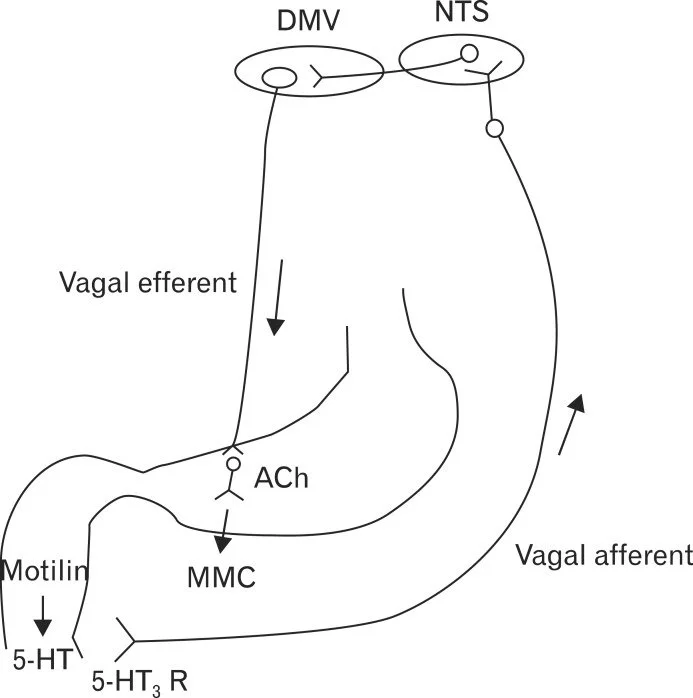
The MMC is a series of contractions that sweep through the stomach and small intestine during periods of fasting, every 90-120 minutes. Its purpose is to cleanse the stomach and small intestine of undigested food, bacteria, and dead cells and by doing so preventing bacterial overgrowth in the small intestine (SIBO).
The MMC is controlled by the hormones motilin and serotonin along with the vagus nerve. Eating disrupts the MMC cycle and the duration of interruption depends on the caloric content and composition of the meal. Impaired MMC function is associated with conditions like small intestinal bacterial overgrowth (SIBO), irritable bowel syndrome (IBS), and gastroparesis. Stress hormones, poor sleep, and eating too often are the main inhibitors of the MMC.
Since the MMC is active during periods of fasting, it is functionally different from peristaltic activity that’s meant to propel food through the digestive tract.
Both of these actions are behind the frequency of bowel movements. Restoring bowel movements so that you’re having 2-3 day has a massive effect on lowering LPS and indirectly increasing energy production.
Tight junction proteins rely on sufficient energy generation from mitochondria. The inhibition of ATP production leads to the loss of gut barrier function. This is called intestinal permeability aka leaky gut. Mitochondrial dysfunction is associated with intestinal diseases like inflammatory bowel disease (IBD) and colorectal cancer (CRC),
After a meal, small intestinal oxygen consumption doubles to satisfy increased energy needs for nutrient processing. Small intestinal epithelial cells rely on glucose and glutamine for energy production.
In the colon, butyrate (a short-chain fatty acid produced by gut bacteria) is the main energy source for colonocytes and provides the fuel for their mitochondria. A loss of energy production in the colonocytes can lead to oxygen leaking into the colon from arterial blood. Obligate anaerobes can’t exist in the presence of oxygen so as they die the facultative anaerobes increase. This is one cause of dysbiosis.
The active thyroid hormone T3 is critical in signaling mitochondrial energy production and this is why hypothyroidism is often the underlying cause of gut issues like constipation and dysbiosis.
Seed oils, pesticides, animal-based antibiotics and stress hormones will shift the microbiome into a more pathological state.
And, high-fat diets decrease colonic concentrations of butyrate that led to impaired mitochondrial bioenergetics.
Another important feature of the intestines is their mucin layer. The mucin layer is thinner in the small intestine as compared to the large intestine and provides a physical barrier between bacteria and the intestinal lining. A very important type of bacteria resides in the mucin layer to regulate it called Akkermansia Mucinaphila. In the colon, it represents about 3-5% of the total bacterial population. If Akkermansia are destroyed due to oxygen leakage, seed oils or antibiotics, this layer can be reduced. Bacteria will then live directly on the intestinal lining causing immune reactions that effect the whole body.
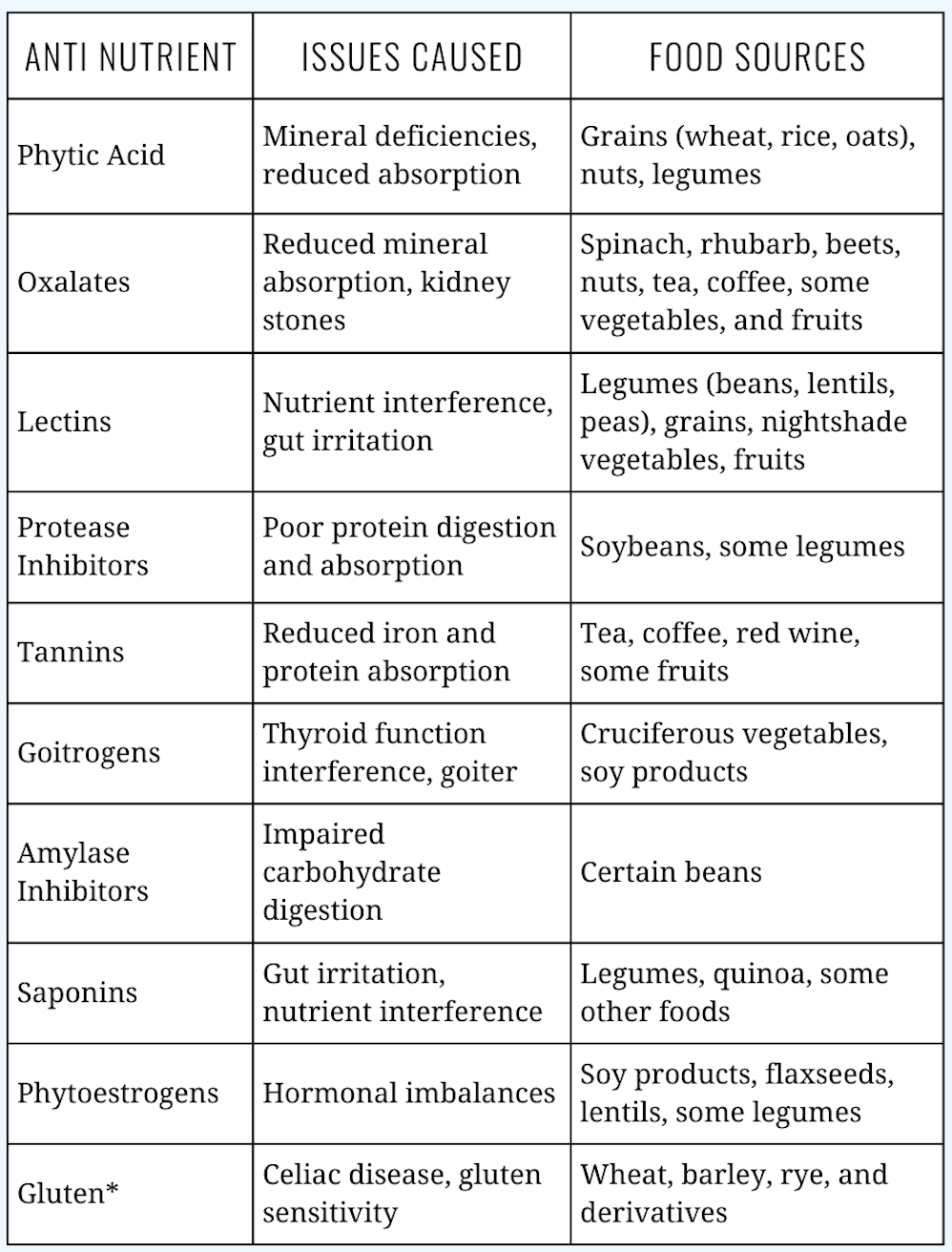
One last consideration in your gut status are plant-defense chemicals. Since plants can’t run or fight, they must defend themselves from microbes, insects and herbivores with chemicals. Sometimes called anti-nutrients, these chemicals are concentrated in leaves, bark, root skins, but in highest amounts in the seeds (plant babies). Seeds in the botanical world are grains, legumes, beans, nuts and seeds.
The function of these defense chemicals can be to irritate the gut lining, prevent nutrient absorption, or straight up poison the consumer. Your response to anti-nutrients is highly unique and will have varying effects depending on your current digestive capacity and microbiome population.
Traditional cultures knew of the gut disruptions caused by anti-nutrients and worked around them by sprouting, soaking, cooking, and fermenting.
As a general rule, animals and fruit not plants, provide the vitamins and minerals in your diet.
Review of the Main Causes Gut Dysfunction
Omega 6 from seed oils
LPS from overgrowth of gram-negative bacteria
Antibiotics
Glyphosate and other pesticides
Stress hormones
Oxygen leakage from poor mitochondrial function and hypothyroidism
Plant defense chemicals
Next week we’ll discuss digestive function and the role of dietary fiber. See you then.
Jonathan
This is for informational purposes only and should not replace professional medical advice. Consult with your physician or other health care professional if you have any concerns or questions about your health.